The Oxford Coronavirus (Covid-19) vaccine – simplified!
It was uplifting to wake up this morning to some good news about the candidate Coronovirus vaccine from the Jenner Institute at the University of Oxford. The vaccine – known as ChAdOx1 nCoV-19 or AZD1222 holds some promise. The paper published yesterday in the Lancet is free to view and I have attached it below for those of you who have a background in the life sciences.
What is so special about ChAdOx1 nCoV-19?
Many of you will know a few basic things about vaccines as we all would have received them at some time. The Jenner Institute in Oxford is appropriately named after Edward Jenner, who is widely regarded as the father of vaccines and immunology. He famously discovered that innoculation with cow pox confers immunity against smallpox – a devastating viral infection with high mortality rates. Although he discovered this in 1796, it was not widely accepted until the UK government passed the Vaccination Act in 1840, providing for free vaccination against smallpox. The last case of small pox was in a three year old Bangladeshi child called Rahima Banu in 1975! Contrast this to the approval of ChAdOx1 nCoV-19 by the Medicines and Healthcare Products Regulatory Authority (MHRA) in 7 days!
 Rahima Banu – the last person with naturally occuring smallpox in 1975.
Rahima Banu – the last person with naturally occuring smallpox in 1975.Copyright: CDC/ World Health Organization Stanley O. Foster
 Edward Jenner (1749-1823) pioneer of the world’s first vaccine. Copyright: Wellcome Gallery
Edward Jenner (1749-1823) pioneer of the world’s first vaccine. Copyright: Wellcome Gallery
The smallpox vaccination was a simple concept. Smallpox is due to the variola virus. Edward Jenner discovered that innoculation with a related virus called vaccinia (which causes cow pox) induced immunity against smallpox. Hence the term “vaccination” is derived from the word vacca – latin for cow.
Since then, many vaccines have been developed. Some are inactivated viruses that are injected to stimulate immunity, others are weakened (attenuated) viruses that do the same. The polio vaccines are examples of vaccines that are available both as an inactivated vaccine or a live attenuated vaccine. The latter is said to produce more lasting immunity at the risk of causing polio in some people.
The Oxford vaccine – ChAdOx1 nCoV-19 – is a very different type of vaccine. It is essentially a modified cold virus that affects chimpanzees. This virus is an adenovirus hence the name ChAdOx1 – chimpanzee, adenovirus, Oxford! ChAdOx1 nCoV1 has been engineered with the genetic instructions to produce the ‘spikes’ that the coronavirus exhibits. The virus itself does not cause an infection in humans but looks like the SARS-CoV2 coronavirus that causes COVID-19. This stimulates the immune system to mount an immune response against the coronavirus.
Kickstarting the immune system
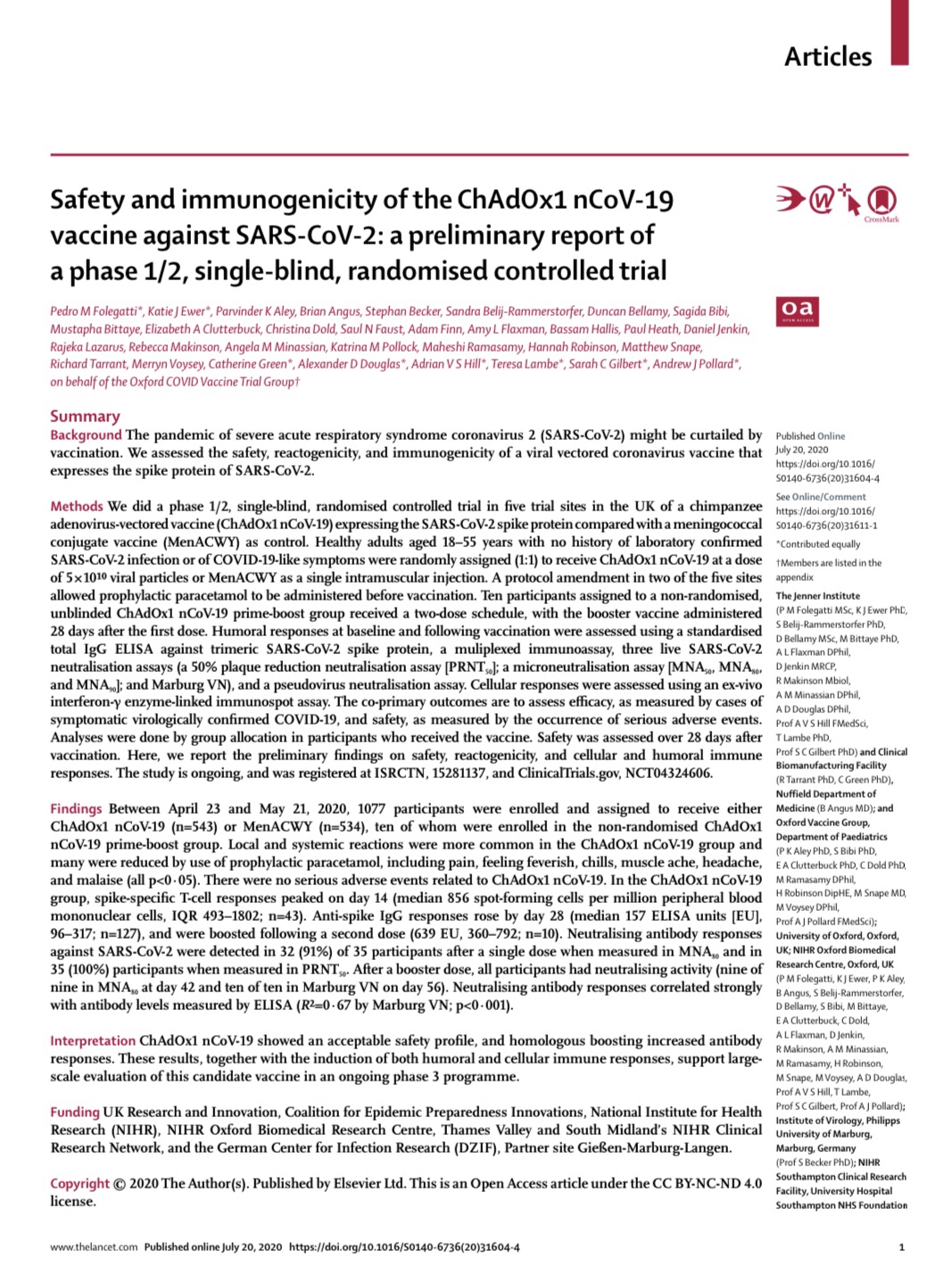
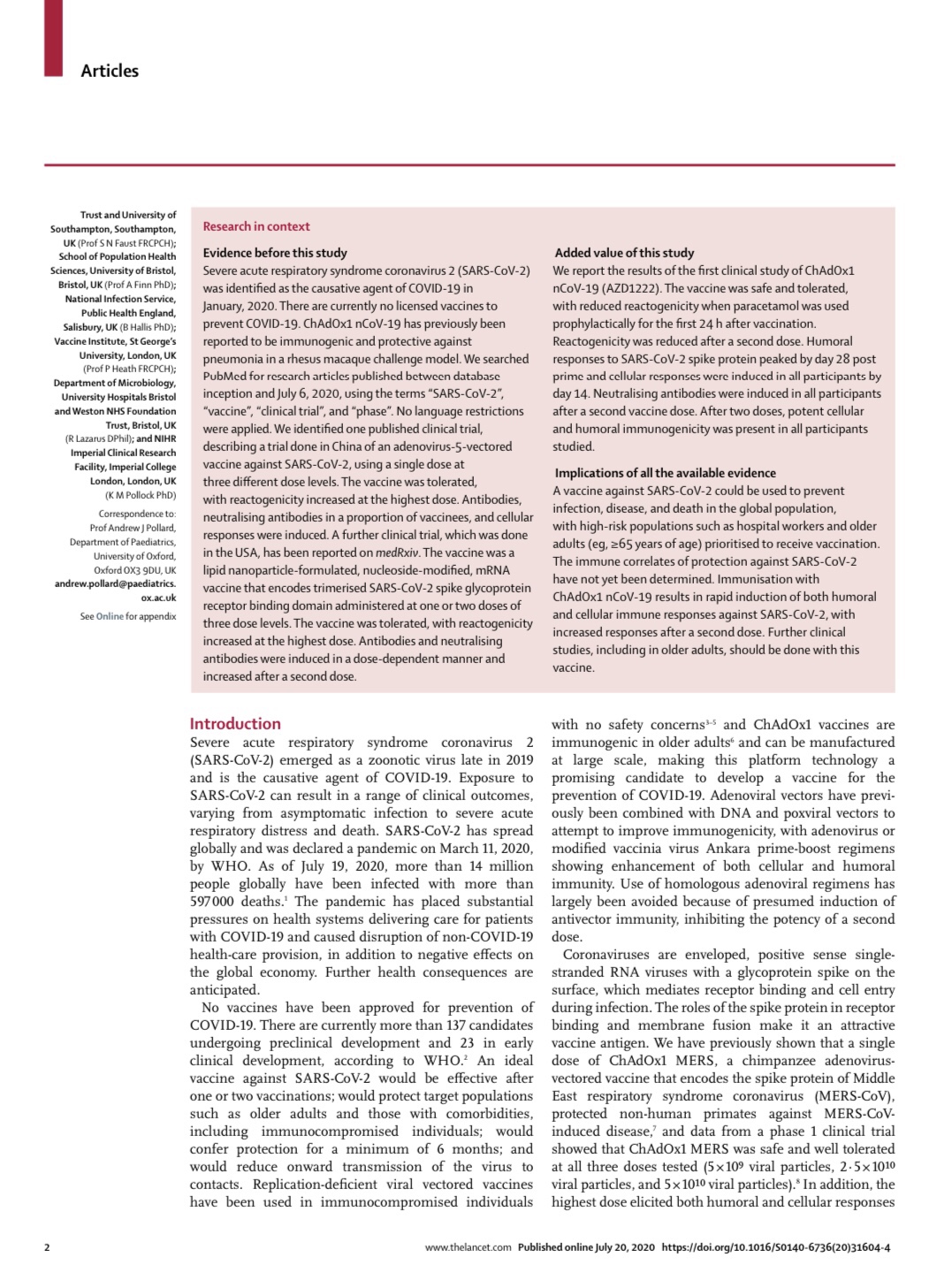
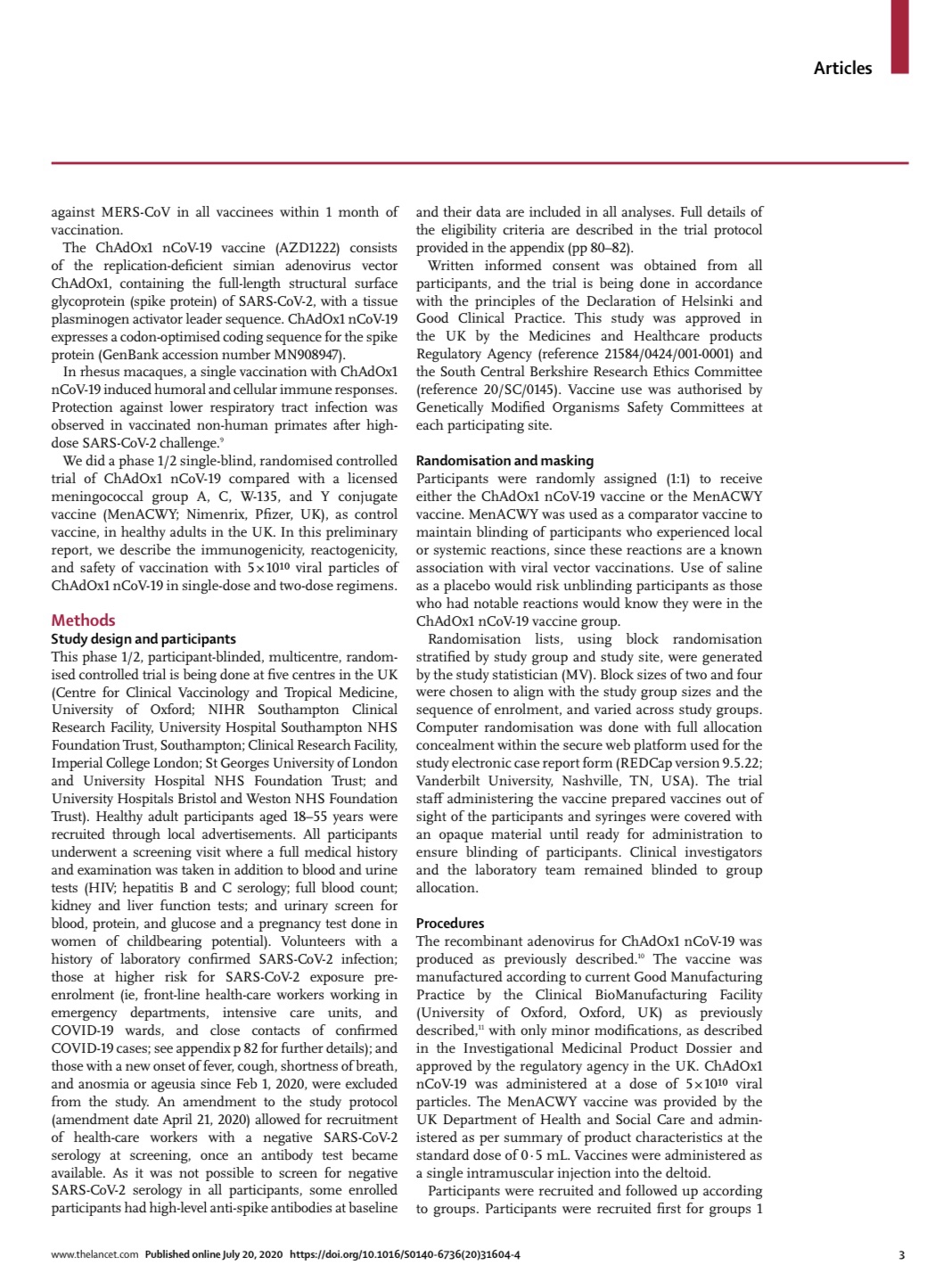
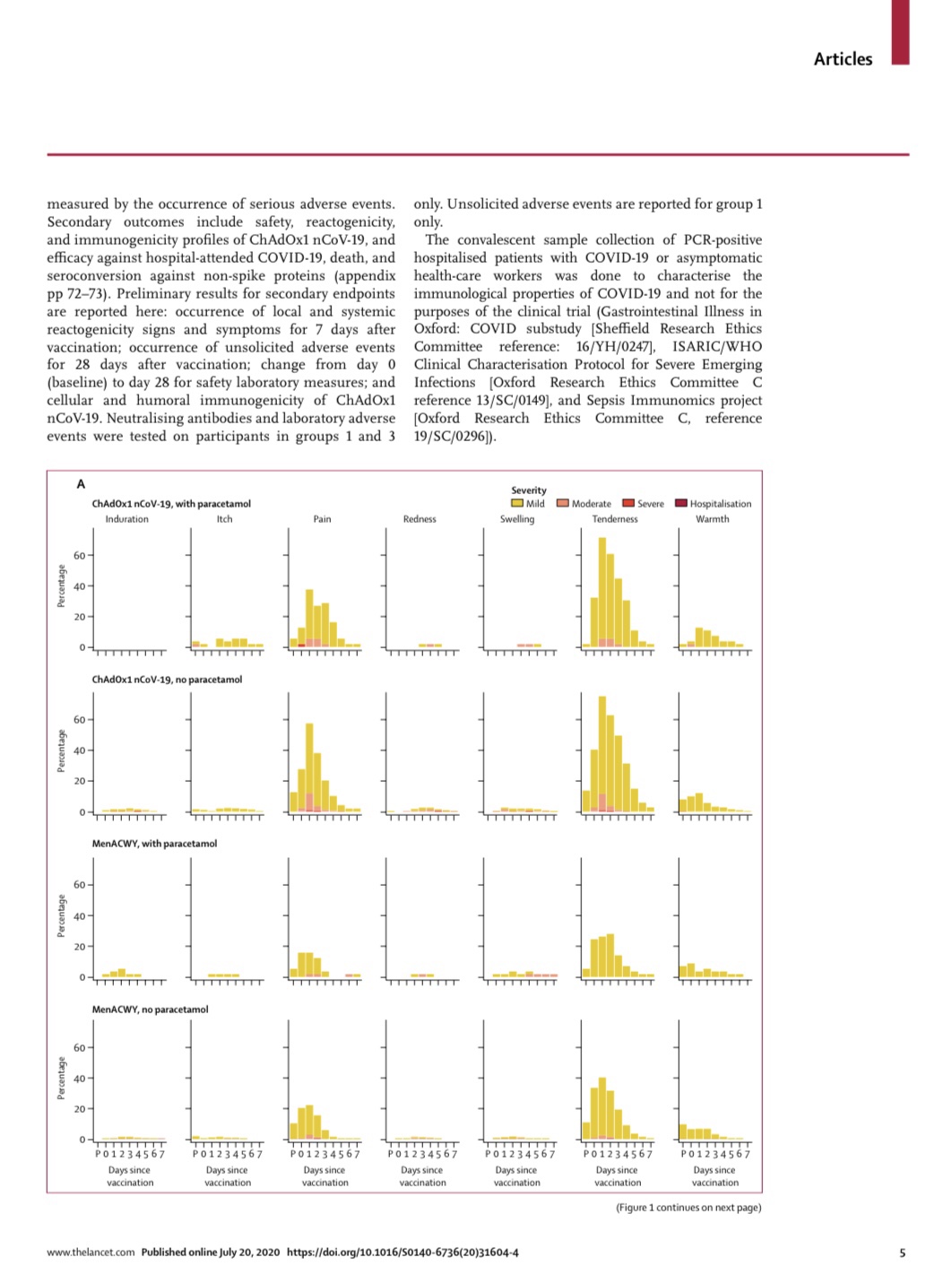
The human immune system is made up of antibodies and also white blood cells that fight infections. A good vaccine not only produces antibodies (humoral immunity) but also stimulates the production of specific white blood cells – called T cells (cellular immunity) – that can identify a virus and destroy it. If a vaccine only stimulates the production of antibodies but not T cells, it is less likely to be effective.
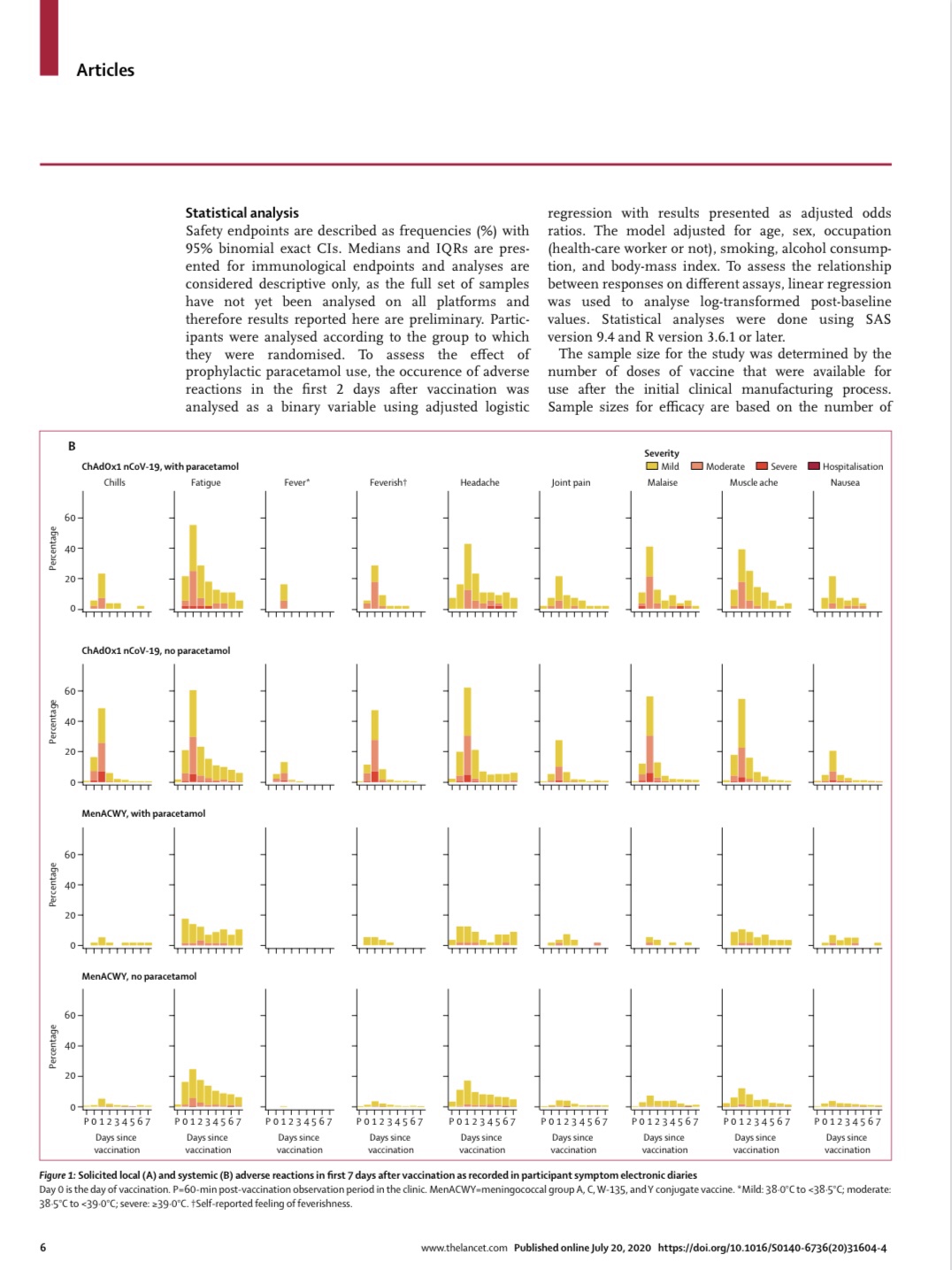
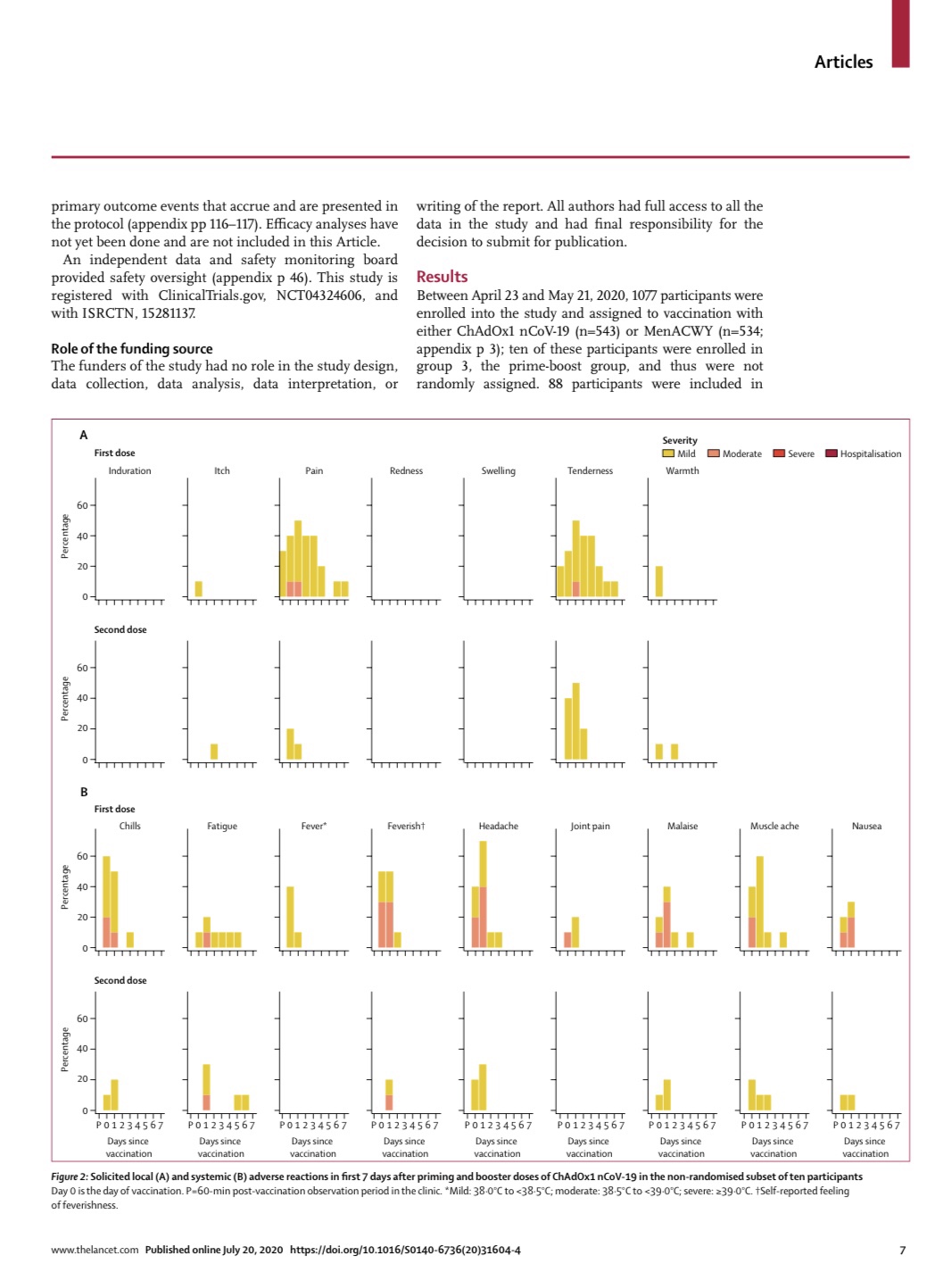
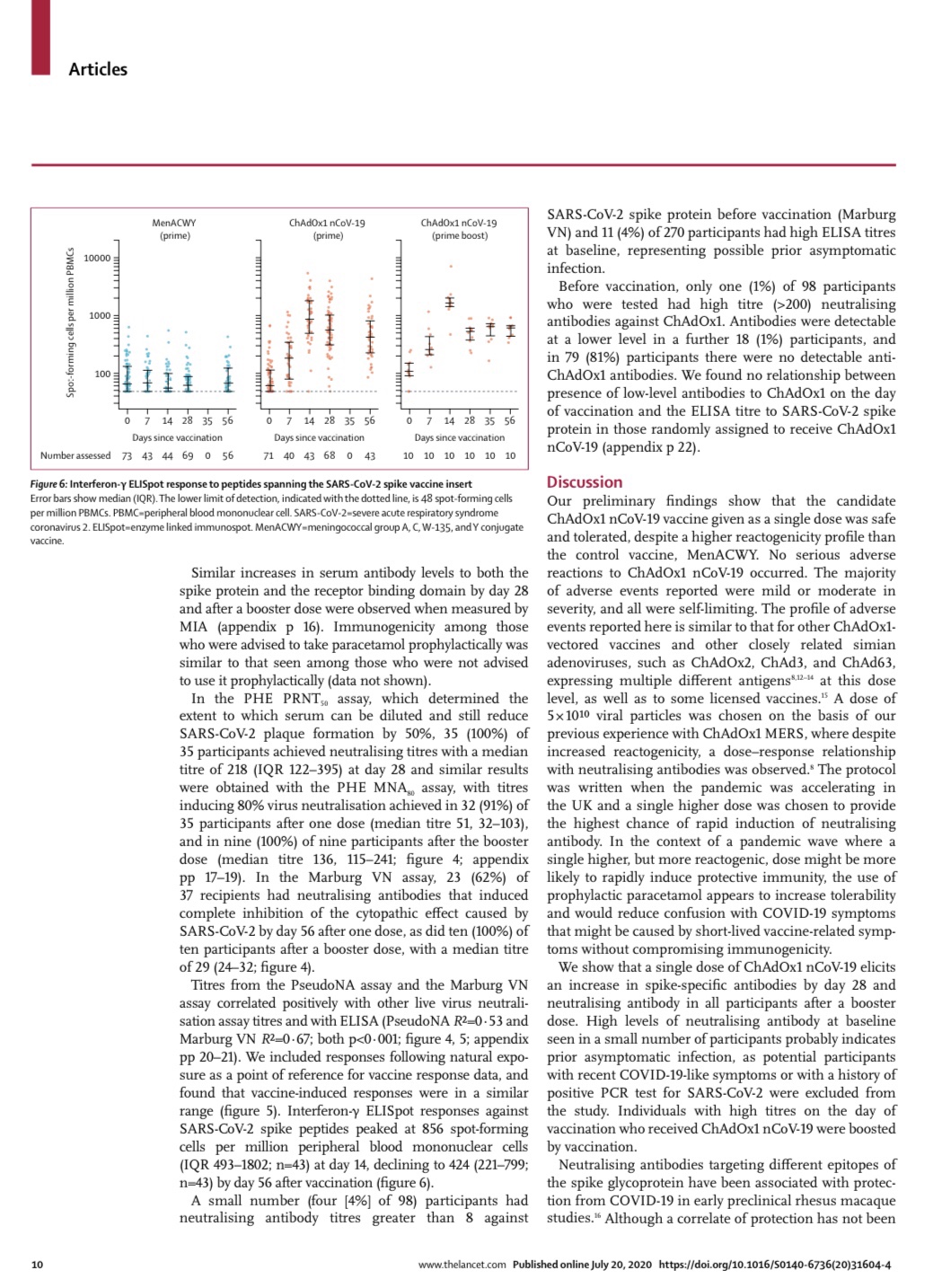
In the recent Lancet study, ChAdOx1 nCoV-19 produces specific nCoV-19 T cells 7 days after vaccination and levels peak at day 14. Antibodies levels rose and peaked at day 28. So ChAdOx1 nCoV-19 appears to stimulate both humoral and cellular immunity. All patients who received 2 doses of the vaccine developed immunity.
The optimistic view ahead
ChAdOx1 nCoV-19 (AZD1222) is now undergoing phase three trials in the UK, Brazil and South Africa. If these go well, the vaccine may be available towards the end of the year. AstraZeneca is working with GAVI (the Vaccine Alliance) and also the Serum Institute of India to ensure that the vaccine will be widely available to all who need it – no matter where they are. One can only hope this becomes a reality and that in 2021 we will be able to eradicate Covid-19!
The pessimistic view ahead
There has never been an effective vaccine against a coronavirus. There are many viral infections that are very well studied – not least HIV – for which we have failed to develop a vaccine. So it is best to be guarded about the prospects of ChAdOx1 nCoV-19 being the panacea to this pandemic. The Lancet study included persons aged 18-55. We know that Covid-19 is most lethal in those older than 55. The study also had very few participants from ethnic minority groups in the UK – 90.9% were white.
Keep calm and let the science lead us
There are 23 vaccines in advanced stages of development. Hopefully a few will become available in the not too distant future. In the mean time, we all need to listen to the science of this disease and allow the experts to lead us out of this morass. One can only hope that the vaccine or vaccines that are of proven value are widely available to all, and do not become a pawn of unscrupulous politicians
 Dinner with my fellow Oxford medics on 16 April 2016 – 20 years after we graduated. Many are frontline doctors in the UK
Dinner with my fellow Oxford medics on 16 April 2016 – 20 years after we graduated. Many are frontline doctors in the UK




Share this blog via:







