Parotid gland tumours and parotidectomy (Warning: Graphic surgical videos in article)
The parotid salivary gland is one of the major salivary glands in the neck. It produces half the total volume of saliva. It is estimated that the two parotid salivary glands produce 0.05 mls per minute of saliva during rest. When chewing and eating, these glands produce up to 3 mls of saliva a minute.
The parotid salivary gland lies in front and below the ear, over the cheek, and angle of the jaw. It is made up of a larger superficial lobe and a smaller deeper lobe. The facial nerve which supplies movement to the face runs between these two lobes. The course of the facial nerve and its branches through the substance of the parotid salivary gland places them at risk during surgery to remove the parotid gland or parotidectomy.
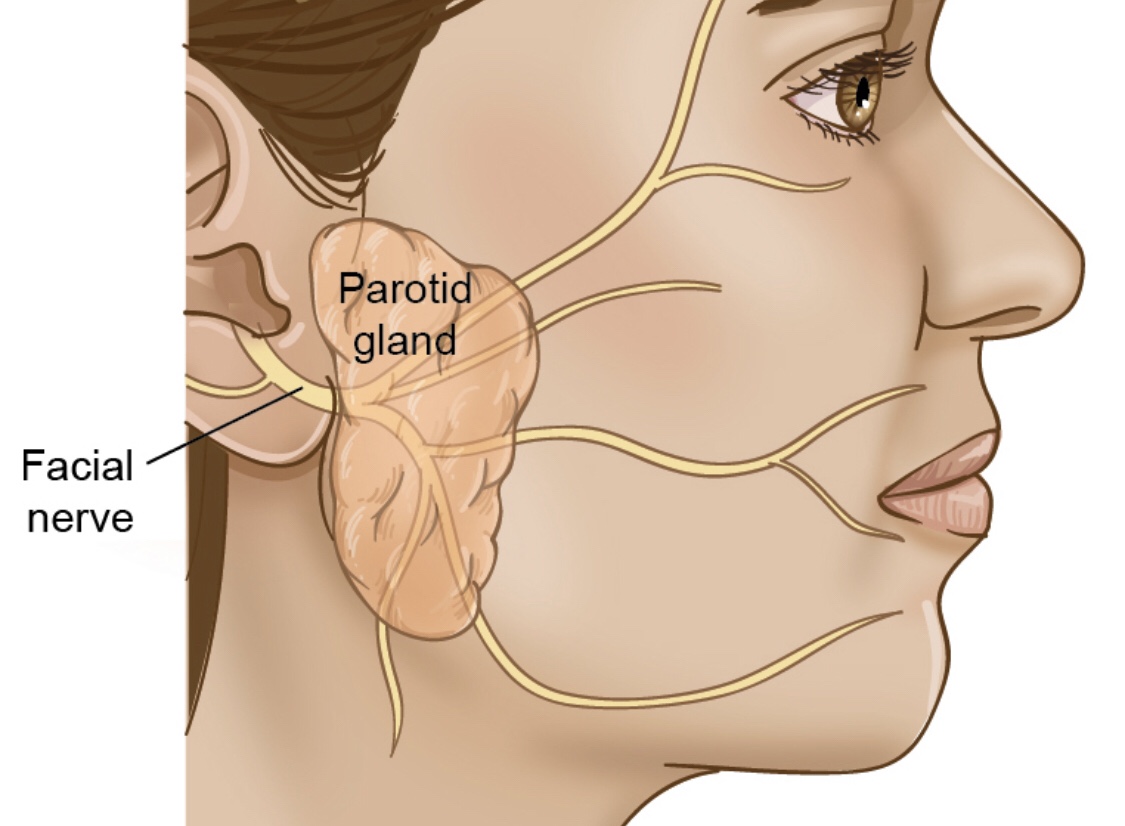
The parotid salivary gland and facial nerve. From Head and Neck Cancer Guide
Tumours of the parotid gland commonly occur in adults. In children, tumours are rare but congenital abnormalities, such cysts, and lymph nodes which arise as a result of infections are common. In Singapore, salivary gland cancers have an incidence of 0.5 to 0.8 per 100,000 population per year. Parotid gland cancers make up 70% of all salivary gland cancers in Singapore. In the years 2008-2012, Singapore saw 30 parotid gland cancers per year amongst its residents.
Tumours of the parotid gland often cause few symptoms. The patient often presents with a painless swelling over the angle of the jaw or cheek. In fact, a painful swelling is less likely to be a tumour and may be due to a stone within the salivary duct causing obstruction or an abscess. The notable exception to this rule is a tumour called a mucoepidermoid carcinoma. These tumors contain cystic spaces and when fluid from these cysts leak out into the parotid gland they may cause pain and inflammation.
Malignant parotid tumours may invade the facial nerve and causing facial paralysis. This often suggests that the tumour is at an advanced stage.
Benign parotid gland tumours
The most common benign tumour of the parotid gland is called the pleomorphic adenoma. It said that 80% of tumours in the parotid gland are benign and 80% of these are pleomorphic adenomas. Pleomorphic adenomas are slow-growing parotid tumours that may turn into cancer. The rate of cancerous (or malignant) transformation is low. Some authors suggest 1% whilst others quote a 9.5% rate over 15 years. When these benign pleomorphic adenomas become cancer they are known as carcinoma ex-pleomorphic adenoma. These cancers are aggressive with only 50% of patients surviving 5 years or more after treatment.
Pleomorphic adenomas of the parotid tend to arise in the superficial lobe of the parotid gland. These tumours have small projections from their surface or pseudopodia which can give rise to recurrent tumour if incompletely removed during surgery.
The other common benign parotid tumour is a Warthin’s tumour or papillary cystadenoma lymphomatosum. These tumours are benign and often seen in elderly men who smoke. In 6% of cases, there may be multiple tumours. Often these tumours can only be definitively diagnosed after removal.
Malignant parotid gland tumours or Parotid Cancer
There are many types of parotid cancer. The low-grade parotid cancers may behave like benign tumours. The more aggressive high-grade ones grow rapidly and can cause paralysis of the face. The most common parotid cancer is a mucoepidermoid carcinoma. These can be classified as low, intermediate, or high-grade cancers.
The other common type of parotid cancer includes adenoid cystic carcinomas which are difficult to eradicate completely and tend to spread along nerves (perineural invasion). Adenocarcinomas which arise from the glandular cells of the salivary gland make up the other large sub-type of parotid cancer. These can be sub-divided into acinic cell carcinomas, polymorphous low-grade adenocarcinomas, basal cell adenocarcinomas, clear cell carcinomas, cystadenocarcinomas, sebaceous adenocarcinomas, sebaceous lymphadenocarcinomas, and mucinous adenocarcinomas
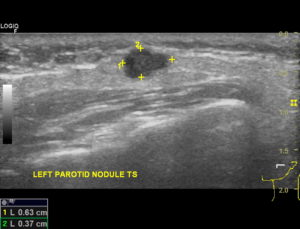
Surgery is often necessary to treat benign and malignant parotid tumours. In fact, in some centres, needle biopsies to confirm the nature of the tumour is often thought to be unnecessary. In our practice, we routinely undertake fine needle biopsies of parotid tumours under ultrasound guidance. We believe knowing the likely nature of the tumour helps with surgical planning.
Parotidectomy
Parotidectomy is surgery to remove the parotid gland. The most common operation done is the removal of the superficial lobe of the parotid. This is called a superficial parotidectomy. When the entire parotid gland is removed, the operation is called a total parotidectomy. The term total conservative parotidectomy has been used to describe operations in which the facial nerve is preserved.
They are various approaches to the parotid gland, but the most common one is through a facelift incision. The skin over the face and cheek is raised exposing the superficial lobe of the parotid gland. Once this is done, the next step is the careful identification of the facial nerve. The use of a nerve monitor ensures that the facial nerve and its branches are protected. Once the root of the facial nerve has been identified, all its branches are traced out and the superficial parotid gland containing the tumour is removed.
Total parotidectomy involves removing the deep lobe of the parotid gland which lies deep to the facial nerve and its branches. In some cases, the lymph nodes in the upper neck are removed together with the parotid gland. This operation is called a neck dissection.
A superficial parotidectomy often takes two hours. Operations that require a total parotidectomy and extensive neck dissection may take five hours. Following surgery, a surgical drain is placed and secured. This drain serves to remove any residual blood in the parotid bed. These drains often remain in the neck for 1 to 2 days.
What can I expect after parotidectomy?
Parotidectomy is not a painful operation. In fact in some cases, patients notice numbness over the cheek and ear lobe. This is due to traction or transection of the great auricular nerve.
These are some of the consequences following surgery:
- Bleeding or a blood clot underneath the skin (haematoma)
- Infection
- Facial weakness
- Salivary collection (sialocoele)
- Frey’s Syndrome (a condition where eating causes a patient to start sweating over the cheek)
- First bite syndrome
Share this blog via: