Coronavirus (Covid-19) and ENT
The Coronavirus or Covid-19 Pandemic will probably register as the single most important world event in my life time. Its effects will last decades and it will fundamentally change the way we live and work. Ear, nose and throat (ENT) surgeons are very much in the frontline of this infectious disease. Although much airtime is given to infectious disease specialists and emergency department physicians, the rise of asymptomatic patients with mild ENT symptoms has highlighted that ENT surgeons are highly likely to see Covid-19 patients and be exposed to high viral loads of the coronavirus when we examine patients. The death of an ENT surgeon in Wuhan early this year and the death of a Consultant ENT Surgeon in United Kingdom last weekend highlight the risks that a simple ENT examination entails.
 Amged El Hawrani, a Paediatric ENT Surgeon working in Queen’s Hospital, Burton-on-Trent, was the first NHS doctor to die in the UK. Photo courtesy of ENT UK
Amged El Hawrani, a Paediatric ENT Surgeon working in Queen’s Hospital, Burton-on-Trent, was the first NHS doctor to die in the UK. Photo courtesy of ENT UKI was particularly touched to read what Amged El Hawrani’s 18 year old son, Ashraf had said about his father – “He taught me the significance of respect and equality. He also stressed the importance of not worrying about the things I cannot control, which he displayed to me right up until the end of his life. He did not seek the praise and approval of others, he was satisfied by viewing the positive effects of his actions and the wellbeing of his family. I am incredibly proud to say that for 18 years of my life, Amged El-Hawrani was my father.”
ENT is the biological epicentre of the Coronavirus
Covid-19 is caused by the SARS-CoV2 coronavirus. The initial reports from Wuhan suggested that the virus is only spread by direct contact and droplet transmission. Droplets are respiratory secretions (nasal mucus or saliva) and are produced when people cough or sneeze. Droplet particles are 5-10 micrometres in size and droplet nuclei are less than 5 micrometres. The coronavirus under normal circumstances is carried and survives in drop particles. So one has to be within a metre of someone with Covid-19 who is sneezing or coughing to pick it up. However, in some circumstances, the coronavirus can survive in droplet nuclei. The presence of the virus in droplet nuclei suggests that airborne transmission is possible. These droplet nuclei can remain in the air for hours and spread beyond 1 metre.
Research has found that certain procedures that generate aerosols can produce droplet nuclei that carry the coronavirus. Simply put, some procedures can lead to airborne transmission of the coronavirus. These procedures include many procedures that ENT surgeons undertake such as nasal endoscopy, voice surgery (endoscopic laryngeal microsurgery or microlaryngoscopy) and tracheostomy. In Wuhan, sinus surgery (specifically trans-sphenoidal pituitary surgery) was undertaken in a patient who was Covid-19 positive unbeknownst to the surgeons and operating theatre staff. The use of powered instruments such as debriders and drills can generate aerosols. Consequently, at least 14 members of the operating team, including individuals outside the operating room contracted Covid-19.
The coronavirus infects the upper airway in humans before progressing to cause a pneumonia. In a paper published in the New England Journal of Medicine in March 2020, the viral load in the nose was compared with that in the throat. Samples of nasal secretions had in the initial phase of the disease a much higher viral load than in the throat.
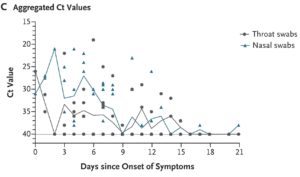 Viral load in nasal swabs compared to throat swabs. In the first few days of symptoms, the viral load in the nose is much higher. Many patients with mild symptoms may well visit their ENT during this period
Viral load in nasal swabs compared to throat swabs. In the first few days of symptoms, the viral load in the nose is much higher. Many patients with mild symptoms may well visit their ENT during this periodTo reduce the risks to surgeons and staff, most ENT clinics like ours are donning Personal Protective Equipment (PPE) when we perform what are termed aerosol generating procedures. Whenever possible, surgery which is not urgent is deferred.
Loss of smell and taste is a symptom of Covid-19
Several weeks ago, my medical school classmate and now illustrious Professor of Rhinology at King’s College, London – Prof Claire Hopkins – described that a large number Covid-19 patients appear to have lost their sense of smell or taste. The loss of smell or anosmia is a common consequence of any viral infection. Indeed about 40% of all patients with anosmia have had a viral infection. Of these, about 15% are due to one of the many coronviruses that affect humans. Prof Hopkins drew on data from Korea, Italy and Germany and suggested that many hitherto asymptomatic Covid-19 positive patients actually had some degree of anosmia.
More recently, a study of 500 Britons who were Covid-19 positive found that 60% had anosmia but only 32% had fever. This casts serious doubt on the value of temperature screening at entry points into airports, offices, schools and hospitals. Perhaps what we need is a simple smell identification test to screen for Covid-19. I now wake up very morning and ensure that I can smell my morning coffee. A truly reassuring aroma!
How Covid-19 has changed ENT practice
The coronavirus pandemic has changed how we practise ENT. All our patients are thoroughly screened before we accept appointments. In Singapore, we are still seeing patients who seek ENT care whether urgent or not. This may soon change if community spread worsens. Already all patients who have a fever, cough or breathless are directed to emergency departments or public health preparedness clinics (PHPCs). These three symptoms are very common is a host of other ENT conditions. Emergency departments and PHPCs do not have the time to treat non-Covid-19 ailments so these patients often come back to us with a normal chest X-ray report and a negative Covid-19 swab test.
The problem is that the sensitivity of the Covid-19 swab test is between 60-70%. What this means is that the test can only detect 2 out of 3 truly positive patients. Or in other words a third of patients will go undetected! The chest X-ray can also be normal in positive patients. These patients then come to an ENT clinic and their negative tests gives everyone a fall sense of security.
All this means ENT surgeons have to assume that all patients we see may have Covid-19. We need to take the necessary precautions to protect ourselves and our staff.
The consultation now is tense and tedious. Patients see us behind face masks and goggles. Conversations are no longer relaxed, history-taking is directed and full of closed-ended questions! The very approach that is frowned upon in most medical schools.
We gown up in PPE before the most simple examinations and disinfect all equipment, examination chairs and work surfaces between patients.
How will it all end?
The more we know about Covid-19, the more we realize how little we actually know. The pandemic is evolving rapidly and advice on how to avoid transmission is also changing. Face masks were deemed unnecessary for those who are not ill, but this advice may soon change as asymptomatic spreaders become the main vector for transmission. We can however beat this pandemic by employing the few facts we know. The coronavirus doesn’t travel, people do. So social distancing and movement restriction must now be the way we live.
Let’s pray that this will soon pass without too heavy a toll. Once it has passed, the world and ENT will be very different, and hopefully a safer place for us and our children.
Stay safe!
Share this blog via:







