Should my child have a tonsillotomy instead of a tonsillectomy?
“Tonsillotomy offers a less painful, safer and equally effective alternative to Conventional Tonsillectomy in treating Sleep Apnoea in children. “
Tonsil enlargement and Obstructive Sleep Apnoea (OSA)
Enlarged tonsils are a common problem in childhood. Large tonsils obstruct the airway and cause noisy breathing and snoring. In some children, large tonsils can completely obstruct the airway and cause the child to stop breathing at night. This condition is called obstructive sleep apnoea (OSA) and may manifest in a variety of ways. These include difficulty waking up, daytime sleepiness, irritability and hyperactivity, poor school performance, and growth retardation.
Surgery for Obstructive Sleep Apnoea (OSA)
Surgical removal of the tonsils (tonsillectomy) and adenoids (adenoidectomy) is an effective treatment for obstructive sleep apnea in children over the age of two. It cures 80-90% of children with this condition. The improvement in a child’s well-being is staggering, with many parents reporting that the child is a completely different child after surgery.
Of the two procedures, tonsillectomy is associated with more pain and a greater risk of complications. Adenoidectomy is largely painless, and the risk of bleeding is much lower.
Conventional or Total Tonsillectomy has been practised for the best part of a century. The advent of general anaesthesia allowed for patients to be completely anaesthetised and their airway secured with an endotracheal tube. The surgeon could then remove the tonsils in their entirety without the patient gagging. The dissection was often “subcapsular”. The tonsil bed was left often to heal by “granulation”. During the period, pain would last 7-10 days, normal diet would only resume after 4-5 days, and there was a risk of bleeding up to two weeks following surgery.
Tonsillotomy or Intracapsular Tonsillectomy
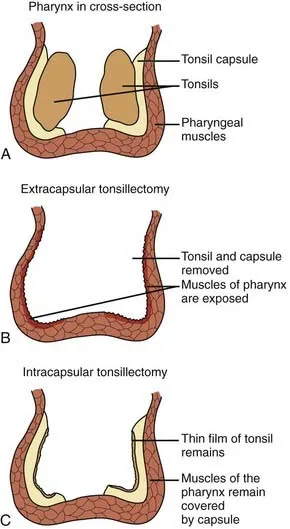
Since 1993, some surgeons have been proposing partial tonsillectomy as an alternative to conventional total tonsillectomy to treat obstructive sleep apnoea in children. The term “tonsillotomy” has been used to describe partial tonsil surgery, where the bulk of the tonsil is reduced so that it no longer protrudes into the airway past the tonsillar pillars. Some surgeons remove tonsillar tissue down to the tonsillar capsule, taking care not to breech this capsule. This is termed intracapsular tonsillectomy.
Diagram from basicmedicalkey.com demonstrating the difference conventional subcapsular tonsillectomy and intracapsular tonsillectomy
What are the benefits of tonsillotomy or intracapsular tonsillectomy?
- Quicker return to normal diet – most children return to a normal diet after 2 days.
- Less pain – typically lasts 3-4 days as opposed to 7-10 days following conventional tonsillectomy.
- Reduced requirement for pain relief medication.
- Fewer episodes of post-tonsillectomy bleeding – the rate for bleeding following conventional tonsillectomy is 4.6%, with 1.8% requiring a return to the operating theatre to stop bleeding. In tonsillotomy, bleeding occurred in 1.3%, with only 0.3% requiring a return to the operating theatre.
What are the disadvantages of tonsillotomy or intracapsular tonsillectomy?
There is a 6% risk of regrowth of tonsillar tissue following tonsillotomy. In most cases, the recurrence does not cause a relapse of sleep apnoea. This means most recurrences are of little to no consequence.
Is tonsillotomy or intracapsular tonsillectomy as effective as conventional tonsillectomy in treating obstructive sleep apnoea (OSA)?
Most studies to date have shown no difference in the efficacy of tonsillotomy or intracapsular tonsillectomy in treating obstructive sleep apnoea. Some long-term studies that have followed patients for 6-10 years also show no relapse of obstructive sleep apnoea.
Are patients with recurrent tonsillitis suitable for tonsillotomy or intracapsular tonsillectomy?
At present, evidence is lacking to recommend tonsillotomy over conventional tonsillectomy in treating children who have recurrent tonsillitis. The number of children who suffer recurrent tonsillitis has been declining over the decades. Indeed, several decades ago tonsillectomy was more commonly done for recurrent tonsillitis. These days, tonsil surgery is more often undertaken for obstructive sleep apnoea.
How is tonsillotomy or intracapsular tonsillectomy performed?
There are several different ways to perform a tonsillotomy. The Microdebrider (shaver), Carbon Dioxide (CO2) laser and Coblation are common instruments used. I prefer Coblation. We are fortunate to have the Werewolf Coblation System at The ENT Clinic. I use the EVAC70 or the Procise EZ View wand. The video below is a 5-minute clip of the surgery.
Is tonsillotomy widely accepted?
Tonsillotomy or intracapsular tonsillectomy is growing in acceptance in most developed countries. It is widely practised in the United States, United Kingdom, Sweden, Germany, France and Australia.
If your child requires tonsil surgery, ask your ENT surgeon if tonsillotomy is an option for him or her.
Dr Jeeve Kanagalingam
Share this blog via: